Recovery from after effects of Covid 19 infections
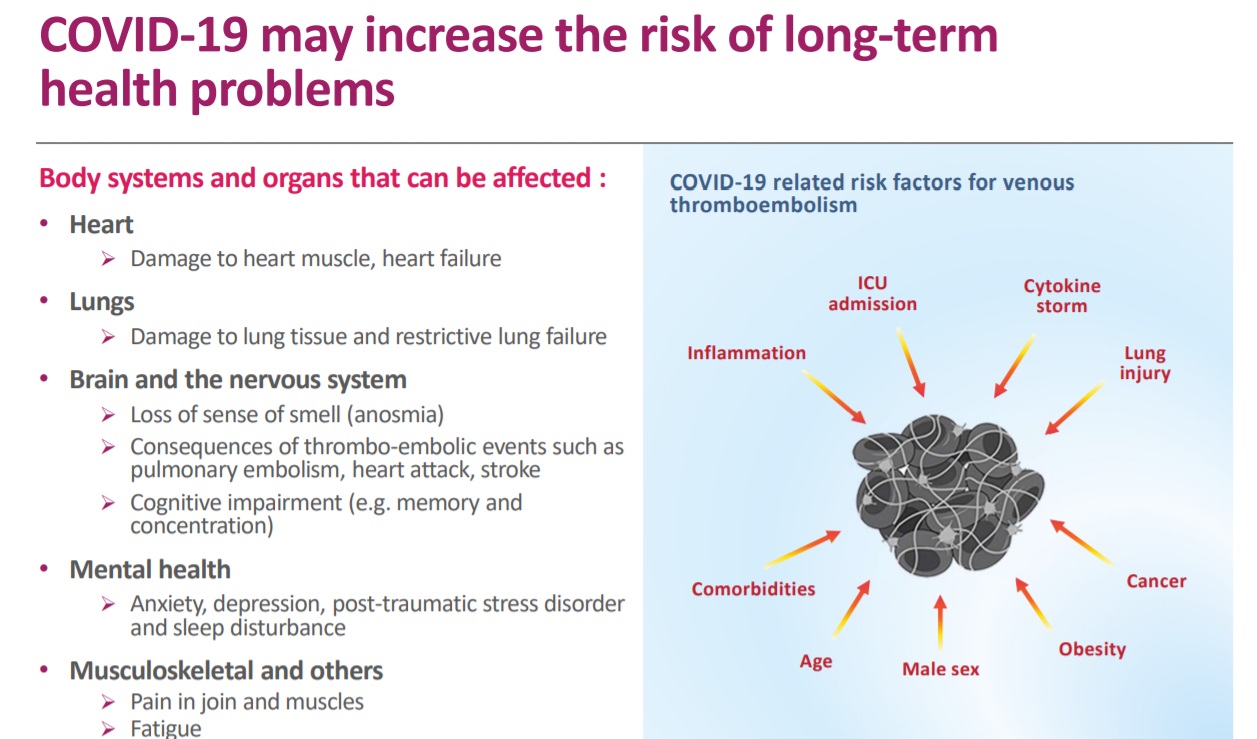
Surviving COVID-19 has been only part of the triumph for some patients. While doctors were well aware of the impact of lasting viral infections, the first few months of the pandemic were devoted to preventing transmission and figuring out how to take care of those in hospitals, and not much attention was paid to the after-effects. But experience over the last 5 months in India have indicated that after effects of Covid 19 can no longer be ignored. Though SARS-CoV-2 is essentially a virus that hits the lungs, in a smaller subset, it also seems to have an impact on the lungs, heart and brain, increasing the risk of long-term health issues, and life-threatening complications.
With 22,057,685 coronavirus cases across the globe and 7, 77,535 fatalities (as at August 2020), the pandemic is still raging in many parts of the world. Even as doctors and medical experts across the globe continue to learn more about the novel coronavirus with every passing day, there is still no clear answer to the long-term implications of COVID-19. It has been more than 8 months since the novel coronavirus first erupted in China and since then it has been established that the disease attacks the entire body. As COVID-19 is a novel disease and vastly different from a regular viral fever, there are not enough studies which underline the long-term effects of the disease.
What kinds of complications may occur?
The good news is that most people who have the novel coronavirus disease recover completely within a few weeks. Some, including even those who had mild versions of the disease, however continue to experience adverse side effects symptoms after their initial recovery. Even people who tested positive but were asymptomatic during the course of their disease are not immune either from long-term effects. It can be tough to get back on your feet post-recovery. With COVID, long-lasting fatigue, weakness (which could persist for weeks and months) has been a much-feared consequence. Not only has COVID-fatigue been much widely discussed by experts, but nearly 60% of the patients involved in the study also admitted to suffering from fatigue, lethargy, tiredness in the weeks following recovery. Of these, 1/3rd, who suffered from a critical form of COVID termed their fatigue to be moderate or severe.
Apart from this, unbalanced energy levels could also expose patients to experience related symptoms like muscle aches, pins and needles pain, palpitations. Improper immune response and inflammatory attack (dubbed the infamous cytokine storm in COVID terminology) has been considered to be one of the causes of energy loss and imbalance.
The list of organs that may be affected by COVID-19
Getting back to normal after COVID 19
Getting back to normal after COVID-19 can take some people a few months. But things usually improve over time.
- Physical problems after COVID-19
- Muscle weakness and joint stiffness
- Extreme tiredness (fatigue) and a lack of energy
- Reduced mobility
- Breathlessness
- Phlegm build-up
- Weaker physical fitness
- loss of appetite and weight loss
- lack of sense of smell or taste
- Stomach problems - this includes heartburn, diarrhoea and vomiting
- Difficulties in swallowing
- Mental and emotional problems after COVID-19
- Sleep problems - this can often develop after being in hospital, where it can be difficult to sleep
- Problems with mental abilities – for example, not being able to remember some events, think clearly and being forgetful
- Changes in mood, or depression or anxiety
- Nightmares or flashbacks
- Post-traumatic stress disorder (PTSD)
- Confusion or delirium
Suffering a severe illness and spending time in hospital can be extremely stressful. Aged persons suffer very often from the above aftereffects. Some people recover from COVID-19 quickly and do not need much support. Other people will need more time and help. Your recovery time could depend on the level of treatment you got in hospital. It can take months to fully recover. Everyone is different. It's important not to compare yourself to others. Having good and bad days during your recovery is normal. It's OK to feel this way.
- Muscle weakness and joint stiffness
- Extreme tiredness (fatigue) and a lack of energy
- Reduced mobility
- Breathlessness
- Phlegm build-up
- Weaker physical fitness
- loss of appetite and weight loss
- lack of sense of smell or taste
- Stomach problems - this includes heartburn, diarrhoea and vomiting
- Difficulties in swallowing
- Sleep problems - this can often develop after being in hospital, where it can be difficult to sleep
- Problems with mental abilities – for example, not being able to remember some events, think clearly and being forgetful
- Changes in mood, or depression or anxiety
- Nightmares or flashbacks
- Post-traumatic stress disorder (PTSD)
- Confusion or delirium
What can help quick and Proper recovery from side effects of Covid 19
Patients who have successfully recovered from the acute COVID-19 pneumonia will require health support to define and quantify the consequences of the disease. Even after discharge from a hospital a recovered Covid patient should be monitored for the following conditions;
Physical conditions:
- Adjust expectations: It’s quite natural for memory and concentration issues to come up after being unwell, so don’t beat yourself up about not being able to get back to your old life and abilities immediately. Take your time, give your mind and body a chance to recuperate.
- General weakness: Covid recovered patients do not bounce back to their previous state of health as soon as they get discharged from the Covid hospital. As they have just fought a ravaging illness and it is better to get into their routine activities gradually, rather than just diving straight in. It is important to prioritise the most important tasks and leave everything else. Covid recovered patients should save body energy as much as possible and postpone unnecessary tasks for a later date. Do not get into rigorous and tough physical action at least for 3 weeks. Covid recovering patients need rest, but gently and gradually introducing them back into your daily life will make you both physically and cognitively stronger.
- Look out for warning signals: Whether it is a nagging headache or a bout of breathlessness, it is important to pay attention to any warning signs that the body is not doing okay. A recovering patient should inform the doctor if any such issues crop up, post-recovery.
- Covid recovered patients with comorbidities: If the recovering patient has any chronic illness like Diabetes, Hypertension or COPD or cardiac illness or stroke and if the patient is on take regular medication for the same, it is strongly advised to monitor the vital parameters like blood pressure, sugar levels, creatinine levels etc preferably under a qualified hospital and ensure that the healthcare provider checks the correctness of vital parameters and revises the dosage as per the need of the hour.
- Balanced nutritious diet: Diet is a very important component of the recovery process. The recovering patient should eat fresh and easy to digest freshly cooked soft diet.
- Continuing Covid Precautions: While contracting COVID-19 may have given your body a certain degree of immunity from the disease, emerging studies have suggested that it is most likely temporary. Hence, continue wearing face covers or face masks in public places and practise social distancing.
Brain & Psychology related recovery activities:
- Prompt yourself: Lists, notes, alarms and reminders can prompt you to get back to activities which you might be missing out on due to brain fog. These can also help you create a routine, which is one of the best ways to feel in control and get back to normal life.
- Brain exercises: Start new activities or hobbies that stimulate the brain, like puzzles, word games, number games, memory exercises and reading. Start with exercises which are achievable, and gradually challenge yourself to increase acuity.
- Break it down: Remembering or concentrating on all the steps of a complicated action might be difficult, so break down the steps and take them one at a time. The prompts mentioned above can come in handy here too.
What is to be monitored in the recovery Phase?
- Cardiac condition: During Post Covid recovery phase, it is essential to check cardiac condition twice a day for 2 weeks. This is especially required to be done for senior citizens and for those who suffer from comorbidities.
- Lung condition: Even after a discharge from a Covid hospital the recovered person might suffer from breathlessness on account of Phlegm build-up. Hence lung condition has to be monitored twice a day. If need be administration of medical oxygen is perhaps required for some patients. Even a repeat HRCT is required to be done for some. In case of Phlegm build-up, it may to be suctioned with a suction apparatus.
- Fluid and Diet Intake: The patient must recover from run down through good fluid intake. This is apart from nutritious diet. Some patients exhibit continued problems of inability to taste and smell. Some will have problems in swallowing. Right type of assistance has to be provided to patients which includes feeding through Riels tube.
- Blood parameters: Parameters like CBP, CRP, LFT, Creatinine, D Dimer, LDH Ferritin and IL 6 are to be monitored in patients who have suffered a run down from Covid 19 infections.
- Physical Support: Recovered patients suffer from severe muscular pain and they require help of attendants for their mobility. If support is not availed a fracture on account of a fall could aggravate the situation.
- Physical therapy: Physical therapy or Physiotherapy provided by a qualified Physiotherapist will go long way in reducing body pain and improves the mobility of recovering patients.
- Continuous review of Medicine prescription: Patients with comorbidities and are recovering from Covid take medicines for pre-existing diseases and also medicines related to recovery from Covid. A hypoglycaemic attack, at the time of recovery from Covid